RCM
How Technology Enhances Modern RCM in Healthcare
What’s Included
- How automation (RPA) streamlines the front-to-back RCM flow
- How AI/NLP improves coding accuracy
- How real-time analytics & dashboards track key RCM metrics
- How digital patient tools (e-statements, text-to-pay, portals
- How payer rule engines & prior-auth tools prevent denials upfront
- How EHR integration, APIs, and secure cloud platforms
Featured Post
The Top Denial Reasons by Insurance Payers and How to Boldly Outsmart Them
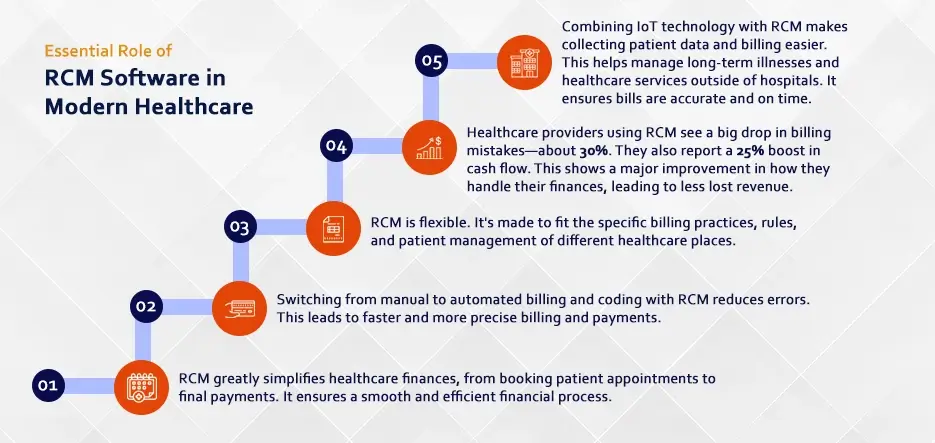
Healthcare practices that cling to paper-based billing and manual processes are leaving millions on the table while their tech-savvy competitors collect faster, reduce costs, and scale effortlessly. The difference between thriving and struggling practices often comes down to one factor: their willingness to embrace modern revenue cycle management technology.
Over the past decade, technology has revolutionized healthcare revenue cycle management, transforming it from a manual, error-prone process plagued by delays and inefficiencies into an automated, data-driven system that maximizes collections while minimizing administrative burden.
Modern RCM technology solutions can dramatically improve your practice’s financial performance, reduce staff workload, and enhance patient satisfaction. From automated claims processing to AI-powered denial prevention, patient engagement platforms, and emerging technologies such as machine learning and predictive analytics, technology is reshaping every aspect of the healthcare revenue cycle.
This comprehensive guide will show you exactly how these innovations work and why they’re essential for your practice’s financial future.
How Technology Transformed RCM
The traditional medical billing RCM process was a nightmare of inefficiency. Claims were printed on paper, mailed to insurance companies, and processed manually. Follow-up required phone calls that often led to busy signals or endless hold times. Denials arrived weeks later via mail, and the appeals process could drag on for months.
This manual approach created massive inefficiencies. Error rates on paper claims often exceeded 30%, meaning nearly one in three claims required rework. Days in accounts receivable regularly stretched beyond 60-90 days, creating cash flow crises for practices of all sizes.
The shift to electronic health records (EHRs) and revenue cycle management systems marked the beginning of a digital transformation. Electronic claims submission reduced error rates to below 10% almost immediately. Real-time eligibility verification prevented coverage issues before they became denials.
Today’s RCM systems integrate seamlessly with EHRs, practice management platforms, and patient engagement tools. This integration creates a unified workflow where patient data flows automatically from registration through final payment without manual intervention.
The ROI comparison is striking. Practices using automated RCM medical billing processes report 40-60% reductions in administrative costs, 25-35% improvements in collection rates, and 50-70% decreases in days in accounts receivable compared to manual processes.
Error rates tell an even more compelling story. Manual claims processing typically results in 20-30% of claims requiring rework. Automated revenue cycle management reduces this to 3-5%, dramatically improving cash flow and reducing administrative burden.
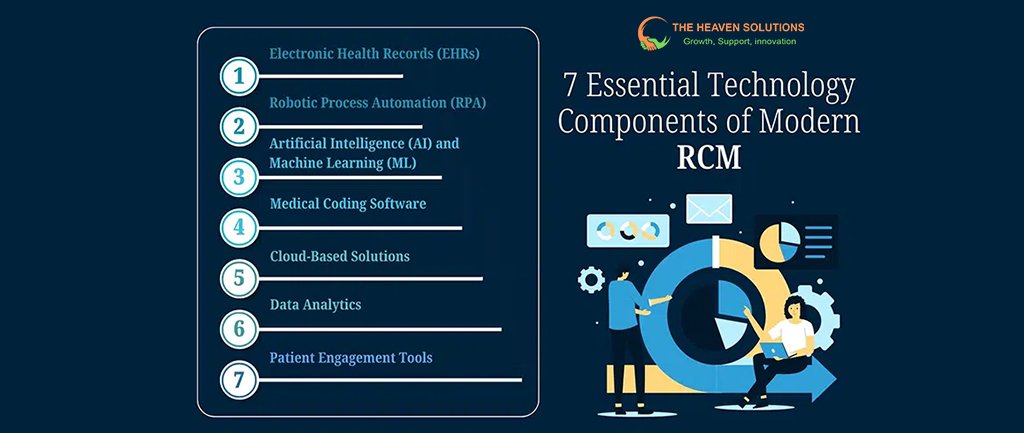
Essential Tools for Modern RCM Success
Modern healthcare RCM relies on an integrated technology stack that automates and optimizes every aspect of the revenue cycle process. Understanding these core technologies helps practice owners make informed decisions about their RCM investments.
Practice Management Systems: The Central Hub
Today’s practice management systems serve as the central hub for all RCM in medical billing activities. These platforms integrate patient scheduling, registration, clinical documentation, and billing into a unified workflow.
Advanced systems include real-time eligibility verification that checks insurance coverage, benefits, and prior authorization requirements before each appointment. This prevents the majority of coverage-related denials and improves the patient financial experience.
Integrated charge capture ensures that all billable services are documented and coded correctly. Built-in compliance checks flag potential coding errors before claims are submitted, dramatically improving clean claim rates.
Claims Processing Technology: Speed and Accuracy Combined
Transforms claims processing from a manual, error-prone task into a streamlined, highly accurate process. Modern claims processing technology includes several critical components.
Real-time eligibility verification happens at every patient touchpoint, from appointment scheduling through service delivery. This ensures that insurance information is current and benefits are verified before services are provided.
Automated claim scrubbing technology reviews every claim against hundreds of payer-specific rules before submission. These systems catch common errors like incorrect patient information, missing modifiers, or coding inconsistencies that typically cause denials.
Electronic claims submission speeds the entire revenue cycle healthcare process. Claims submitted electronically are processed within 24-48 hours compared to 7-14 days for paper claims. This acceleration directly improves cash flow.
Industry benchmarks show dramatic improvements with these technologies. Practices using comprehensive claim scrubbing report clean claim rates of 95-98% compared to 70-80% for those relying on manual processes.
Payment Processing Platforms: Streamlining Collections
Modern payment processing technology automates the most time-consuming aspects of collections. Electronic Remittance Advice (ERA) allows practices to receive payment information electronically, eliminating manual posting of payments.
Automated payment posting reduces the time between receiving payments and updating patient accounts from days to minutes. This real-time updating improves cash flow reporting and reduces billing inquiries from patients.
Practices implementing automated payment posting typically reduce their days in accounts receivable by 10-15 days while decreasing payment posting costs by 60-80%.
Patient Portal Integration: Enhancing Financial Engagement
Patient engagement technology transforms the financial experience for both practices and patients. Online bill pay capabilities allow patients to view statements, make payments, and set up payment plans 24/7.
Patient revenue cycle technology includes cost estimation tools that provide patients with accurate out-of-pocket estimates before services are provided. This transparency improves patient satisfaction while increasing upfront collections.
Automated payment reminders via email and text reduce the need for manual collection calls while improving payment rates. Studies show that practices using automated patient communications see 25-40% improvements in patient collection rates.
How AI Is Revolutionizing Revenue Cycle Management
Artificial intelligence represents the next frontier in RCM technology, offering capabilities that were impossible just a few years ago. AI-powered tools analyze vast amounts of data to identify patterns, predict problems, and automate complex decision-making processes.
Preventing Problems Before They Occur
AI-powered predictive analytics examine historical denial patterns, payer behaviors, and coding trends to identify potential issues before claims are submitted. These systems can predict which claims are likely to be denied and why, allowing staff to address problems proactively.
Revenue cycle management technology
Using predictive analytics typically reduces denial rates by 20-35% compared to reactive denial management approaches. The financial impact is substantial – a practice with $2 million in annual charges could save $100,000-200,000 annually through improved denial prevention.
Machine learning algorithms continuously improve their accuracy by analyzing outcomes and refining their predictions. This means the technology gets smarter and more effective over time.
Reducing Errors and Improving Compliance
AI-powered coding assistance tools analyze clinical documentation and suggest appropriate codes based on the services provided. These systems understand the nuances of medical terminology and can identify coding opportunities that human coders might miss.
Accuracy rates for AI-assisted medical coding exceed 95% in many specialties, compared to 85-90% for manual coding alone. This improvement translates directly into higher clean claim rates and faster payments.
Compliance checking features flag potential coding errors, unbundling issues, or modifier problems before claims are submitted. This proactive approach prevents denials and reduces audit risks.
Maximizing Appeal Success
Machine learning algorithms analyze denial patterns and historical appeal outcomes to prioritize which denials are worth appealing and predict success rates. This intelligence helps practices focus their limited resources on appeals most likely to succeed.
Healthcare revenue cycle management
Systems using AI for denial management report 40-60% improvements in appeal success rates compared to manual approaches. The technology identifies the specific documentation or information needed for successful appeals, streamlining the process.
Automated appeals generation creates initial appeal letters based on denial reasons and supporting documentation, reducing the time required to submit appeals from hours to minutes.
Reduced Operational Costs and Increased Focus
AI tools analyze patient data to predict collection difficulties before services are provided. These systems consider factors like insurance coverage, payment history, credit scores, and demographic information to assess financial risk.
Practices using RCM automation for patient financial assessment report 30-50% improvements in upfront collection rates. By identifying high-risk accounts early, staff can implement appropriate collection strategies or payment plans before services are provided.
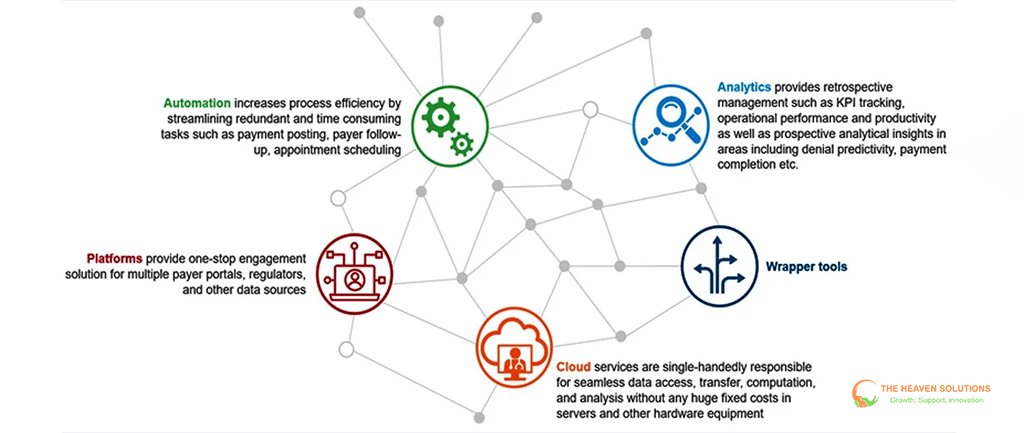
The Power of the Cloud, Scalability, Security, and Seamless Integration
Cloud-based RCM systems offer significant advantages over traditional on-premise solutions, particularly for smaller practices that lack extensive IT resources.
Scalability Benefits: Growing Without Growing Pains
Cloud-based revenue cycle management systems scale automatically as practices grow. Adding new providers, locations, or services doesn’t require hardware investments or complex system upgrades.
This scalability is particularly valuable for practices experiencing rapid growth. Traditional systems often require expensive upgrades or replacements as volume increases, while cloud solutions adjust capacity automatically.
Cost structures for cloud-based healthcare RCM typically include only the features and capacity you actually use, making them more cost-effective for smaller practices while providing enterprise-level capabilities.
Data Security and Compliance: Enterprise-Level Protection
Modern cloud-based RCM technology offers security features that exceed what most practices can implement independently. HIPAA-compliant cloud infrastructure includes encryption, access controls, and audit trails that meet or exceed regulatory requirements.
Security breach statistics show that cloud-based systems are significantly more secure than on-premise solutions. Major cloud providers invest millions in security infrastructure that individual practices could never afford.
Automated backups and disaster recovery capabilities ensure that practice data is protected and accessible even during emergencies. This reliability is crucial for maintaining revenue cycle operations during unexpected disruptions.
Real-Time Reporting and Analytics: Insights Anywhere, Anytime
Cloud-based systems provide instant access to key performance indicators and financial metrics from any location. Practice owners can monitor RCM metrics in real-time, whether they’re in the office, at home, or traveling.
Advanced analytics capabilities help identify trends and opportunities that might not be apparent from traditional reports. Interactive dashboards allow users to drill down into specific metrics and understand the factors driving performance.
Integration capabilities connect cloud-based RCM services with existing EHRs, practice management systems, and patient engagement platforms, creating a unified technology ecosystem.
How Technology Improves the Patient Financial Experience
Modern revenue cycle management technology extends far beyond internal processes to enhance the entire patient financial experience. These improvements benefit both patients and practices by reducing confusion, improving satisfaction, and accelerating collections.
Digital Payment Solutions: Convenience Drives Collections
Mobile payment options allow patients to pay bills using smartphones, tablets, or computers. QR codes on statements can instantly connect patients to secure payment portals, eliminating the friction of traditional payment processes.
Contactless payment options became essential during the COVID-19 pandemic but continue to provide value through improved convenience and reduced processing costs.
Patient satisfaction surveys consistently show preferences for digital payment options over traditional billing methods. Practices offering comprehensive digital payment solutions report 35-50% higher patient satisfaction scores related to billing processes.
Financial Counseling Tools: Transparency Builds Trust
Cost estimation calculators provide patients with accurate out-of-pocket estimates before services are provided. These tools consider insurance benefits, deductibles, and coinsurance to give patients realistic financial expectations.
Real-time benefit verification ensures that cost estimates are based on current insurance information, reducing surprises and billing disputes. Patients appreciate knowing their financial responsibility upfront rather than receiving unexpected bills weeks later.
Healthcare revenue cycle transparency leads to higher upfront collection rates and improved patient relationships. Studies show that practices providing accurate cost estimates collect 60-80% more patient responsibility upfront compared to those that don’t.
Automated Communications: Reducing Administrative Burden
Automated appointment confirmations, payment reminders, and financial notifications reduce the workload on front office staff while improving patient engagement. These communications can be customized based on patient preferences and delivered via email, text, or phone.
Reduction in billing inquiries is a significant benefit of automated patient communications. Practices implementing comprehensive automated communication systems report 40-60% decreases in patient billing questions.
Payment reminder effectiveness varies by delivery method and timing. Text message reminders typically achieve 40-60% response rates, while email reminders achieve 20-30% response rates. Automated phone reminders are most effective for older patient populations.
Emerging Technologies Shaping the Future of RCM
The revenue cycle management technology landscape continues to evolve rapidly. Understanding emerging trends helps practices prepare for future opportunities and avoid obsolescence.
Robotic Process Automation (RPA): Eliminating Routine Tasks
RPA technology automates repetitive, rule-based tasks that currently require human intervention. Examples include data entry, claim status checking, and eligibility verification.
Early adopters of RPA in healthcare revenue cycle management report 50-80% reductions in time required for routine administrative tasks. This automation frees staff to focus on higher-value activities like patient care and complex problem-solving.
Implementation costs for RPA have decreased significantly, making this technology accessible to practices of all sizes. Many RCM service providers now include RPA capabilities as standard features rather than premium add-ons.
Blockchain Technology: Secure and Transparent Transactions
Blockchain creates immutable records of all revenue cycle transactions, from initial service delivery through final payment. This transparency reduces disputes and simplifies audit processes.
Smart contracts on blockchain platforms can automatically execute payment processes when predefined conditions are met, reducing delays and administrative overhead.
While still emerging, blockchain technology shows promise for eliminating many of the trust and verification issues that currently slow healthcare revenue cycle processes.
Voice Recognition and Natural Language Processing: From Speech to Revenue
Advanced voice recognition technology can automatically convert physician notes and dictation into coded, billable services. This automation reduces documentation burden while improving coding accuracy.
Natural language processing analyzes unstructured clinical documentation to identify missed billing opportunities and ensure comprehensive charge capture.
Integration with existing RCM software allows these technologies to enhance current workflows rather than requiring complete system replacements.
Internet of Things (IoT) Integration: Connected Care and Billing
Connected medical devices can automatically capture billable services as they’re performed, eliminating manual charge entry and reducing missed charges.
Remote patient monitoring devices generate billable data continuously, creating new revenue opportunities while improving patient care.
IoT integration with revenue cycle management systems ensures that all billable services are captured and coded correctly, regardless of where they occur.
Technology as a Business Strategy
Modern RCM technology isn’t just about improving efficiency – it’s essential for remaining competitive and financially healthy in today’s healthcare environment. Practices that fail to adopt these technologies find themselves at an increasing disadvantage.
The financial benefits compound over time. A practice improving its clean claim rate from 85% to 95% while reducing days in accounts receivable from 45 to 30 days can improve cash flow by hundreds of thousands of dollars annually.
Patient expectations continue to evolve toward digital-first experiences. Practices that can’t provide online bill pay, cost transparency, and mobile-friendly interactions risk losing patients to more technologically advanced competitors.
Regulatory compliance requirements increasingly favor practices with robust technology infrastructure. Automated audit trails, real-time reporting, and comprehensive data security are becoming table stakes rather than competitive advantages.
The importance of revenue cycle management technology extends beyond financial metrics to operational sustainability. Practices relying on manual processes struggle to attract and retain qualified staff, while those with modern technology can offer more satisfying work environments.
Ready to harness the power of modern RCM technology for your practice? Contact The Heaven Solutions today for a comprehensive technology assessment and customized implementation plan. Our experts will help you identify the right solutions to optimize your revenue cycle, reduce administrative burden, and improve your bottom line. Don’t let outdated technology hold your practice back – embrace the future of healthcare revenue cycle management today.
