RCM
Revenue Cycle Management for Healthcare An Essential Complete Guide
What’s Included
Featured Post
The Top Denial Reasons by Insurance Payers and How to Boldly Outsmart Them
Healthcare providers lose billions annually due to inefficient revenue cycle processes, but the practices that master RCM see collection rates above 95% while their competitors struggle with cash flow crises. The difference between thriving and surviving in today’s healthcare landscape often comes down to one critical factor: how well you manage your revenue cycle.
Revenue cycle management for healthcare
Revenue cycle management for healthcare encompasses everything from patient registration to final payment collection, serving as the financial backbone of healthcare operations. When optimized properly, RCM in healthcare can transform struggling practices into profitable enterprises while improving patient satisfaction and reducing administrative burden.
This comprehensive guide will equip healthcare providers with the knowledge to optimize their healthcare revenue cycle, improve cash flow, and reduce administrative costs. We’ll explore RCM fundamentals, core components, common challenges, optimization strategies, technology solutions, and proven implementation best practices that deliver measurable results.
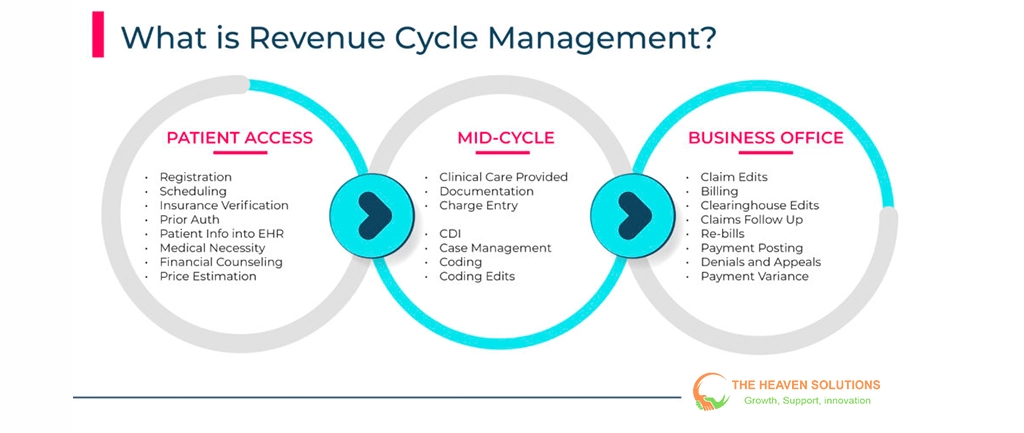
Revenue cycle management is the process that tracks patient care episodes from registration and appointment scheduling to final payment of services. What is RCM in healthcare? It’s a systematic approach to managing all administrative and clinical functions that contribute to capturing, managing, and collecting patient service revenue.
The revenue cycle definition in healthcare extends beyond simple billing. It encompasses patient access, health information management, patient financial services, and business office operations. Understanding what RCM means in healthcare is crucial because it directly impacts every aspect of practice operations and financial performance.
The Financial Impact of Effective RCM
Statistics show that effective revenue cycle management in healthcare can improve collection rates by 15-25% while reducing administrative costs by up to 30%. Practices with optimized RCM systems typically achieve net collection rates above 95%, compared to industry averages of 85-90% for practices with inefficient processes.
The benefits of revenue cycle management extend beyond improved collections. Well-managed healthcare RCM reduces days in accounts receivable from 60+ days to 30-35 days, dramatically improving cash flow. Administrative costs decrease as automated processes replace manual tasks, and staff productivity increases when workflows are streamlined.
Operational Benefits Beyond Finance
Streamlined RCM processes reduce staff workload by eliminating redundant data entry, reducing claim denials, and automating routine tasks. This efficiency improvement allows clinical staff to focus on patient care rather than administrative duties.
Patient satisfaction improves when revenue cycle management includes transparent financial counseling, accurate cost estimates, and convenient payment options. Patients appreciate knowing their financial responsibility upfront and having flexible payment alternatives.
Current Industry Challenges
Healthcare providers face unprecedented challenges that make effective RCM management more critical than ever. Rising patient responsibility due to high-deductible health plans means practices must collect more from patients while maintaining positive relationships.
Complex payer requirements, frequent policy changes, and regulatory compliance demands require sophisticated revenue cycle management systems that can adapt quickly to changing conditions. Manual processes simply cannot keep pace with these evolving requirements.
ROI Considerations
The return on investment for RCM optimization typically pays for itself within 6-12 months. A practice generating $2 million annually in charges can see additional collections of $200,000-400,000 through improved revenue cycle management, while reducing administrative costs by $50,000-100,000.
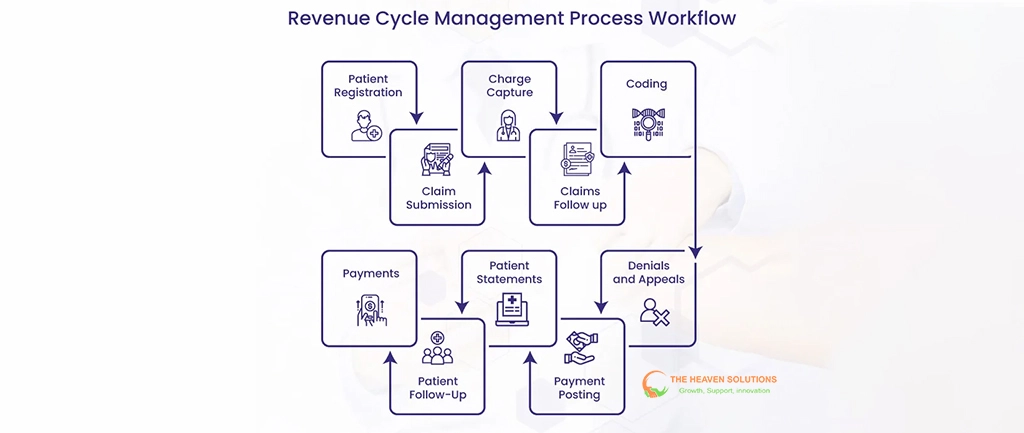
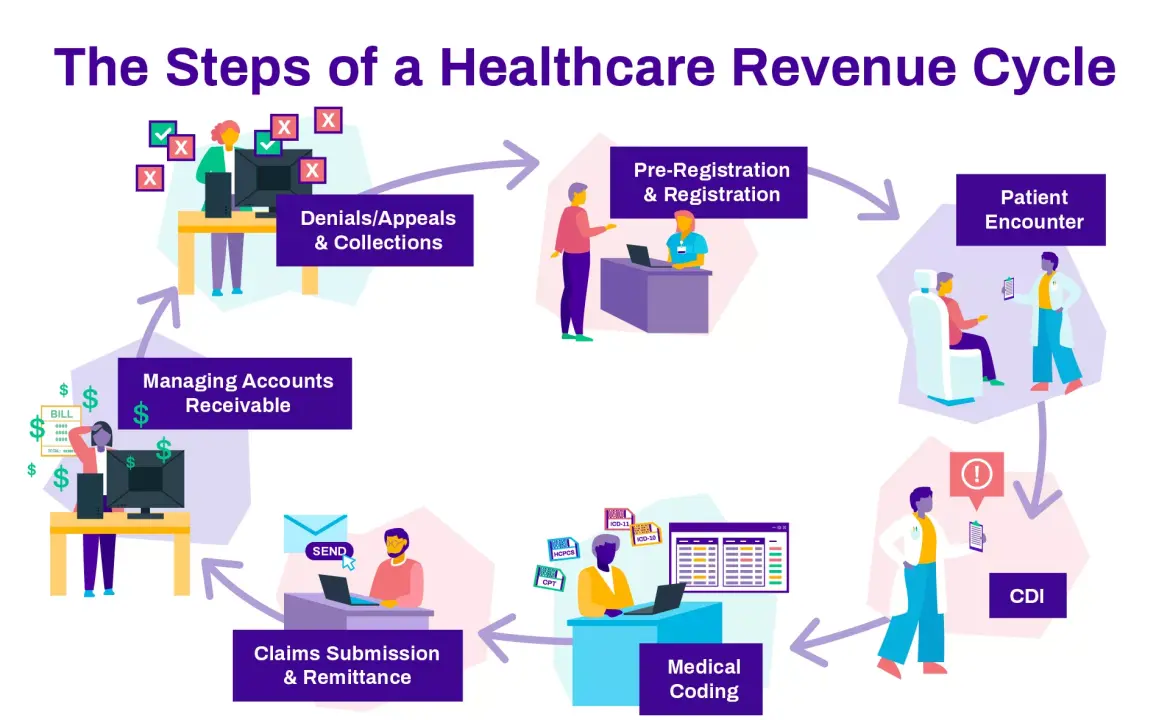
Understanding the steps in the revenue cycle is fundamental to optimization. The healthcare revenue cycle consists of seven critical components that must work seamlessly together to maximize financial performance.
Patient Registration and Scheduling
The revenue cycle begins before the patient arrives for their appointment. Accurate data collection during registration prevents downstream problems that cause claim denials and payment delays. RCM billing success depends on collecting complete demographic information, insurance details, and authorizations.
Real-time eligibility verification ensures that insurance information is current and benefits are active. This verification prevents coverage-related denials that account for 20-30% of all claim rejections in practices without systematic verification processes.
Eligibility and Benefits Verification
Healthcare revenue cycle management requires a comprehensive understanding of each patient’s insurance coverage, including deductibles, copayments, coinsurance, and coverage limitations. Prior authorization requirements must be identified and obtained before services are provided.
Modern RCM systems automate eligibility verification, checking coverage in real-time, and flagging potential issues before they become expensive problems. This automation is essential for practices to maintain high clean claim rates and avoid preventable denials.
Charge Capture and Coding
Proper documentation and accurate medical coding form the foundation of successful medical billing RCM. Every billable service must be captured, coded correctly, and supported by appropriate documentation to ensure optimal reimbursement.
RCM medical billing requires expertise in ICD-10 diagnostic coding and CPT procedural coding, along with an understanding of modifier usage and bundling rules. Coding errors are among the leading causes of claim denials and underpayment.
Clean claims processing is the cornerstone of effective revenue cycle management in medical billing. Claims must be accurate, complete, and submitted according to payer-specific requirements to ensure prompt payment.
Electronic claims submission through RCM software reduces processing time from weeks to days while improving accuracy through automated edits and validations. Practices using electronic submission typically see 40-60% faster payment cycles.
Payment Processing
Efficient payment processing includes electronic remittance advice (ERA) handling, automated payment posting, and reconciliation procedures. Medical revenue cycle management systems automate these processes, reducing manual labor while improving accuracy.
Patient revenue cycle components include patient statement generation, payment plan management, and collection activities. These functions must be integrated with insurance processing to provide comprehensive financial management.
Denial Management
Systematic denial analysis, appeals processes, and root cause identification are essential for maintaining high collection rates. Revenue cycle optimization requires tracking denial patterns and implementing preventive measures to reduce future denials.
Effective denial management protocols can reduce denial rates from industry averages of 10-15% to best-practice levels below 5%. This improvement directly translates to faster cash flow and reduced administrative costs.
Patient Collections
Patient financial counseling, payment plan options, and collection strategies must preserve relationships while maximizing collections. Healthcare revenue management increasingly focuses on patient experience as high-deductible plans shift more responsibility to patients.
Transparent cost estimation and upfront collection strategies improve both patient satisfaction and collection rates. Practices that discuss financial responsibility before services are provided collect 60-80% more patient payments than those that bill after the fact.
Overcoming Revenue Cycle Obstacles: Proven Strategies for Common Healthcare Billing Challenges
Every healthcare practice faces similar RCM challenges, but successful organizations implement systematic solutions that address root causes rather than symptoms. Understanding these common obstacles and proven solutions helps practices avoid costly mistakes.
Technology Integration Issues
Disconnected systems create data silos that increase manual work and introduce errors. Healthcare RCM success requires integrated platforms that share data seamlessly between registration, clinical documentation, and billing systems.
Modern revenue cycle management systems provide APIs and integration capabilities that connect existing EHRs with billing platforms. This integration eliminates duplicate data entry while improving accuracy and workflow efficiency.
Cloud-based RCM solutions offer particular advantages for smaller practices that lack extensive IT resources. These platforms provide enterprise-level capabilities without requiring significant hardware investments or technical expertise.
Staff Training and Retention
Knowledge gaps in coding, billing procedures, and payer requirements create errors that reduce collections and increase administrative costs. Comprehensive training programs address these gaps while building internal expertise.
Revenue cycle management requires ongoing education as regulations, codes, and payer policies change frequently. Successful practices invest in continuous training rather than treating education as a one-time event.
Staff retention strategies include competitive compensation, professional development opportunities, and recognition programs. High turnover in billing departments is particularly costly due to the specialized knowledge required for effective RCM management.
Denial Management Excellence
Proactive denial prevention is more cost-effective than reactive appeals management. RCM systems with built-in edits and validations catch errors before claims are submitted, dramatically reducing denial rates.
Systematic appeal processes with clear timelines ensure that denied claims are worked on promptly and appeals are submitted within required timeframes. Missing appeal deadlines converts potentially collectible revenue into permanent write-offs.
Root cause analysis of denial patterns identifies systematic problems that can be corrected through process improvements or additional training. This analysis is essential for continuous revenue cycle optimization.
Patient Financial Engagement
Improving upfront collections requires transparent financial counseling that explains patient responsibility in clear, understandable terms. Cost estimation tools help patients understand their expected out-of-pocket expenses before services are provided.
Flexible payment options, including payment plans and patient financing, make healthcare more accessible while improving collection rates. Online payment portals provide the convenience that patients expect in other industries.
Patient revenue cycle optimization includes automated payment reminders, digital statements, and self-service options that reduce administrative burden while improving patient satisfaction.
Compliance and Regulatory Requirements
Staying current with changing regulations requires systematic monitoring of updates and implementation of necessary changes. Healthcare revenue cycle management must adapt to new requirements while maintaining operational efficiency.
Audit readiness involves maintaining proper documentation, implementing internal controls, and conducting regular compliance reviews. These activities prevent costly penalties while identifying improvement opportunities.
Risk management protocols include staff training on compliance requirements, regular policy updates, and incident reporting procedures. These systems help practices identify and address potential problems before they become costly violations.
Performance Measurement and Analytics
Establishing KPI tracking systems provides visibility into revenue cycle performance and identifies areas needing improvement. Key metrics include clean claim rate, denial rate, days in A/R, and net collection rate.
Benchmarking against industry standards helps practices understand their relative performance and set realistic improvement targets. RCM analytics reveal trends and patterns that guide strategic decision-making.
Data-driven improvement plans use performance metrics to prioritize initiatives and measure progress. This systematic approach ensures that improvement efforts focus on areas with the greatest potential impact.
Leveraging Technology for RCM Excellence: Modern Tools That Transform Healthcare Revenue Management
Technology transformation is essential for healthcare revenue cycle optimization. Modern RCM software provides capabilities that were impossible with manual processes, including real-time analytics, automated workflows, and predictive insights.
Practice Management Systems Integration
Integrated platforms streamline workflows by connecting patient access, clinical documentation, and billing processes. Revenue cycle management technology eliminates data silos while providing comprehensive reporting capabilities.
Automated routine tasks include eligibility verification, claim scrubbing, and payment posting. This automation reduces manual labor costs while improving accuracy and consistency.
Comprehensive reporting provides real-time visibility into RCM metrics and performance trends. Dashboard interfaces allow managers to monitor key indicators and identify issues requiring attention
AI and Machine Learning Applications
Predictive analytics identify patterns that help prevent denials before they occur. RCM systems using artificial intelligence analyze historical data to predict which claims are likely to be rejected and why.
Automated coding assistance tools analyze clinical documentation and suggest appropriate codes based on the services provided. These systems improve coding accuracy while reducing the time required for manual review.
Intelligent claims processing routes claims based on complexity and likelihood of approval. Simple claims are processed automatically, while complex cases receive human review, optimizing both efficiency and accuracy.
Patient Engagement Platforms
Online portals provide 24/7 access to billing information and payment options. Patient revenue cycle tools include cost estimators, payment plan calculators, and automated communication systems.
Mobile payment options allow patients to pay bills using smartphones or tablets. QR codes on statements provide instant access to secure payment portals, eliminating friction in the payment process.
Automated communication tools send appointment reminders, payment notifications, and educational messages that improve patient engagement while reducing administrative workload.
Cloud-Based Solutions Advantages
Scalable platforms grow with practice needs without requiring hardware upgrades or system replacements. Healthcare RCM solutions in the cloud provide enterprise capabilities at costs accessible to smaller practices.
Security features exceed what most practices can implement independently. HIPAA-compliant cloud infrastructure includes encryption, access controls, and audit trails that meet regulatory requirements.
Real-time access to performance data enables remote monitoring and management. Practice owners can track RCM performance from any location, supporting distributed work environments and multi-location practices.
Integration and Interoperability
Seamless connectivity between EHRs, billing systems, and third-party applications improves data flow while reducing manual entry. Revenue cycle management systems with robust APIs support custom integrations and workflow optimization.
Data standardization ensures that information flows accurately between systems without translation errors or data loss. This standardization is essential for practices using multiple software platforms.
Workflow automation connects processes across different systems, creating end-to-end efficiency that eliminates handoffs and reduces processing time.
Building Your RCM Success Plan: Step-by-Step Implementation for Sustainable Revenue Growth
Successful revenue cycle management transformation requires systematic planning and execution. Organizations that achieve sustainable improvements follow proven implementation methodologies that minimize disruption while maximizing results.
Integration and Interoperability
Seamless connectivity between EHRs, billing systems, and third-party applications improves data flow while reducing manual entry. Revenue cycle management systems with robust APIs support custom integrations and workflow optimization.
Data standardization ensures that information flows accurately between systems without translation errors or data loss. This standardization is essential for practices using multiple software platforms.
Workflow automation connects processes across different systems, creating end-to-end efficiency that eliminates handoffs and reduces processing time.
Change Management Strategy
Leadership buy-in is essential for successful transformation. Practice owners and managers must communicate the benefits of RCM improvements and provide the resources necessary for implementation success.
Staff communication plans address concerns about change while highlighting benefits for individual team members. Successful healthcare revenue cycle management transformations involve staff in planning and decision-making processes.
Training programs provide comprehensive education on new processes and technologies. Adult learning principles guide program design to ensure knowledge retention and practical application.
Phased Implementation Approach
Rolling out improvements systematically minimizes disruption while allowing for adjustments based on early results. Revenue cycle management transformations typically begin with foundational improvements before adding advanced features.
Quick wins provide early success stories that build momentum for larger changes. Examples include automated eligibility verification and claim scrubbing that show immediate results.
Pilot programs test new processes with a limited scope before full implementation. This approach identifies potential issues and allows for refinement before organization-wide rollout.
Training and Support Systems
Comprehensive staff education covers both technical skills and soft skills required for effective patient revenue cycle management. Training programs include hands-on practice with real scenarios.
Ongoing coaching provides individualized support as staff adapt to new processes. RCM management requires continuous learning as systems and regulations evolve.
Performance monitoring tracks individual and team progress while identifying areas needing additional support. Regular feedback helps staff understand their contribution to overall success.
Continuous Optimization Culture
Regular performance reviews compare actual results to established targets and identify opportunities for further improvement. Healthcare revenue cycle optimization is an ongoing process rather than a one-time project.
Benchmark comparisons ensure that practice performance remains competitive as industry standards evolve. External benchmarking provides an objective perspective on improvement opportunities.
Iterative improvements based on data analysis ensure that revenue cycle management continues to evolve and improve. This systematic approach prevents complacency while maximizing long-term results.
Measuring Success: Key Metrics That Matter
Effective RCM requires consistent measurement and monitoring of key performance indicators. These metrics provide objective evidence of improvement while identifying areas needing attention.
Clean claim rate should exceed 95% for well-managed practices. This metric directly impacts cash flow and administrative costs. Days in A/R should remain below 40 days for most specialties, with best-practice organizations achieving 30-35 days.
Net collection rate targets vary by specialty but should exceed 95% for practices with optimized processes. Denial rate should remain below 5% through proactive prevention and systematic management.
Patient satisfaction scores related to billing and financial processes provide insight into the patient experience. Patient collection rates should exceed 80% through transparent communication and flexible payment options.
Your Path to RCM Excellence Starts Now
Revenue cycle management for healthcare is not just about collecting money it’s about creating sustainable financial health that enables you to focus on what matters most: providing excellent patient care. The practices that master RCM don’t just survive in today’s challenging environment; they thrive and grow.
The strategies outlined in this guide provide a roadmap for transformation, but success requires commitment to change and systematic execution. Whether you’re struggling with cash flow, dealing with high denial rates, or simply want to optimize your existing processes, effective healthcare RCM can transform your practice’s financial performance.
Remember that revenue cycle optimization is an ongoing journey, not a destination. The healthcare industry continues to evolve, and successful practices adapt their RCM processes to meet new challenges while maintaining operational excellence.
Ready to transform your practice’s revenue cycle performance? Contact The Heaven Solutions today for a comprehensive RCM assessment and customized optimization plan. Our proven methodologies have helped hundreds of healthcare providers achieve collection rates above 95% while reducing administrative burden.
Benchmark comparisons ensure that practice performance remains competitive as industry standards evolve. External benchmarking provides an objective perspective on improvement opportunities.
Iterative improvements based on data analysis ensure that revenue cycle management continues to evolve and improve. This systematic approach prevents complacency while maximizing long-term results.
