RCM
How to Build an
Essential Denial Management
Workflow That Actually Works
Featured Post
The Top Denial Reasons by Insurance Payers and How to Boldly Outsmart Them
What We offer:
- Why Your Current Denial Management Isn't Working
- The Problem with Reactive Approaches
- Essential Components of an Effective Denial Management Workflow
- Building Your Denial Management Workflow, Step by Step
- Technology and Tools That Support Workflow Success
- Measuring Success and Continuous Improvement

If you’re a healthcare professional juggling claims, you know how much time denial management eats up. In fact, some practices spend nearly a third of their administrative hours just handling denials, usually in a reactive, disjointed way that pushes revenue out the door. If this sounds familiar, chasing your tail over the same denials and feeling like your team can never catch up, you’re not alone.
But denials don’t have to be inevitable. The real challenge is that many organizations approach denial management without a structured workflow. When each denial gets treated as a one-off fire drill, it’s tough to see the bigger picture or make headway on cash flow.
This guide will give you practical steps, insights, and a real-world path for building a denial management workflow that actually works. You’ll learn why common efforts fall short, what essential components your workflow needs, and how to implement a system that protects your revenue and keeps your staff focused on care, not chaos.

Most practices find themselves in a reactive cycle with denial management. It often feels like putting out fires instead of building a fireproof plan. Understanding where common approaches fall short is the first step to lasting improvement.
The Problem with Reactive Approaches
Too often, denial responses are urgent and last-minute: appeals are rushed, staff scramble for documents, and patients grow frustrated over the delays. With no time set aside for big-picture thinking, denial management stays stuck in a loop.
Evidence shows that being reactive can cost practices several times more than a proactive approach, not only in hours but in missed revenue. If you don’t address root causes, you’re forced to keep repeating the same time-consuming work.
Example: A missing prior authorization triggers a denial. Your staff hustle to fix it, but without a prevention plan, the same issue crops up again for the next patient. The cycle drains time and morale, leaving little energy for revenue-generating improvements.
Here’s where RCM (revenue cycle management) comes in. When denial management is siloed and reactive, it disrupts the broader revenue cycle, hurting cash flow, adding stress, and making daily operations harder than they need to be.
The Hidden Costs of Poor Workflow Design
Too often, denial responses are urgent and last-minute: appeals are rushed, staff scramble for documents, and patients grow frustrated over the delays. With no time set aside for big-picture thinking, denial management stays stuck in a loop.
Evidence shows that being reactive can cost practices several times more than a proactive approach, not only in hours but in missed revenue. If you don’t address root causes, you’re forced to keep repeating the same time-consuming work.
Example: A missing prior authorization triggers a denial. Your staff hustle to fix it, but without a prevention plan, the same issue crops up again for the next patient. The cycle drains time and morale, leaving little energy for revenue-generating improvements.
Here’s where RCM (revenue cycle management) comes in. When denial management is siloed and reactive, it disrupts the broader revenue cycle, hurting cash flow, adding stress, and making daily operations harder than they need to be.
The Burden of Administrative Tasks
A denial management workflow that’s unclear or outdated multiplies problems. Staff may create their own workarounds or handle similar denials in totally different ways. Training new hires becomes more difficult with no standardized approach. And each time a seasoned team member leaves, valuable knowledge goes, too.
Inefficiency also drains practice resources. Time spent on “putting out denial fires” could be invested in patient care, staff development, or growth strategies. Good RCM management is about optimizing these revenue cycle steps from patient check-in to final payment for both financial and operational health.
To set up a denial management workflow that truly helps your practice, you need a smart mix of prevention, organization, and accountability. Here’s what matters most:
Prevention and Early Detection Systems
Winning the denial game starts with prevention. Real-time insurance eligibility checks catch issues before they grow into denials. Prior authorization tracking ensures procedures don’t get performed before approvals are in place.
Claims scrubbing and validation before submission let modern RCM systems flag errors, wrong codes, missing data, and ineligible patients so you can fix them before denials happen.
Automated alerts help your team act quickly when something (like expiring coverage or needed referral updates) requires attention. And regular staff education keeps everyone on the same page about what to watch for, so prevention becomes second nature.
Systematic Resolution Processes
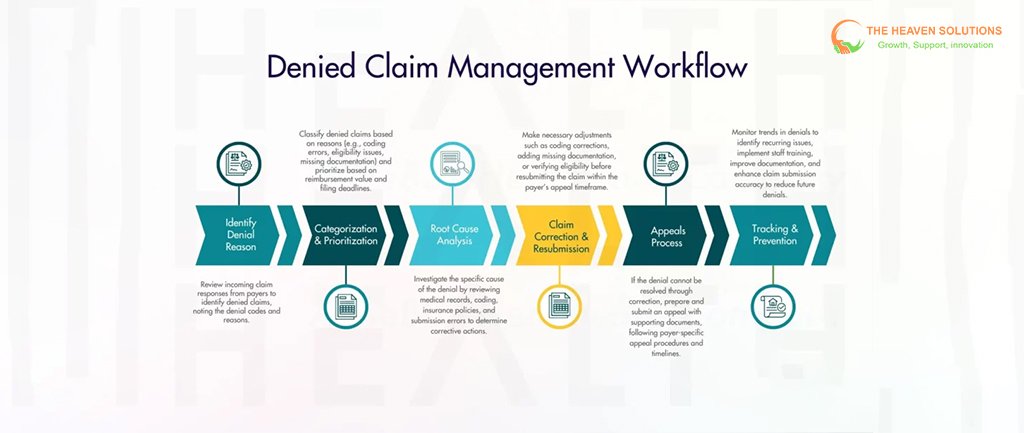
Even with great prevention, denials can still happen. Systematic workflows help you respond efficiently:
- Categorize and prioritize: Which denials are high-value? Which have looming deadlines? Start there.
- Use standardized appeal templates and checklists: This keeps documentation complete and appeals more likely to succeed.
- Assign clear ownership: Every denied claim should have a point person and a clear deadline to move it forward.
- Track progress: Use technology to monitor where each denial is in the process, so nothing goes missing or gets stuck.
Have an escalation plan: Some denials need extra attention, clinical input, or payer follow-up, so have a process ready.
Building Your Denial Management Workflow, Step by Step
A great denial workflow doesn’t happen by accident. Here’s how to build (and refine) yours
Phase 1: Assessment and Planning
Start with a denial audit: Which denials are costing you the most, and why? Spot the root causes, not just the symptom, so you target your efforts effectively.
Set clear, realistic goals and benchmarks. What would success look like? Who needs to be involved? Form a focused team with a variety of perspectives (billing, clinical, admin, IT) to guide the work.
Finally, create a timeline with achievable milestones to keep your project moving.
Phase 2: Design and Implementation
Map your ideal workflow from the moment a denial arrives to full resolution. This helps you see where you might automate or streamline. Standardize your process so all team members handle denials the same way, and set up documentation to keep things organized.
You may need to introduce new RCM systems or upgrade existing ones to support your workflow. Make sure your staff understand not just how to use these tools, but why the new process matters.
Test your process on a small scale before rolling it out to the whole organization. Use feedback to make any necessary tweaks.
Phase 3: Launch and Optimization
Roll out changes in phases by denial type, department, or payer. Track results closely and use regular check-ins to tackle issues early. Gather input from frontline staff about what’s working and what isn’t.
Use metrics to spot bottlenecks and make data-driven improvements. Keep this “continuous improvement” mindset active well after launch, adapting to new regulations and payer policies as needed.
Technology and Tools That Support Workflow Success
Select software that fits your practice’s needs and helps, not hinders, your workflow:
- Automated denial tracking: Lets you categorize and assign claims efficiently.
- Practice management and EHR integration: Seamless data sharing speeds up response times.
- Analytics/reporting: Understand which denials are recurring, and how effective your resolutions are.
- Collaboration tools: Make it easy for team members to follow up or share updates.
- Mobile features: Allow remote work, making the workflow sustainable no matter how your team operates.
Choose tech that supports compliance and security standards, especially when handling sensitive patient information. Look for options that fit your budget and assess return on investment before committing.
Measuring Success and Continuous Improvement
You’ll know your denial workflow is working when you start seeing positive changes in these metrics:
- Denial rates go down.
- Appeal success rates go up.
- Time to resolution decreases.
- Cash flow and revenue recovery improve.
- Staff say the system is manageable and clear.
Regularly audit your workflow. Stay current on new payer guidelines and invest in ongoing staff training. Use performance data to refine the process, scaling it up as your volume increases, so you stay efficient and effective.
Common Pitfalls and How to Avoid Them
Even good plans can stall if you don’t tackle roadblocks head-on:
- Staff resistance: Change is hard. Clearly explain the benefits and take feedback seriously.
- Technology hiccups: Plan carefully for integration with current systems and proper data migration.
- Limited resources: Start with the basics, phasing in more complex elements as time or budget allows.
- Losing momentum: Celebrate early wins and keep communicating the “why” behind the new workflow.
- Over-automation: Use technology for efficiency, but keep people involved for tough, unusual cases.
Sustain your workflow by regularly updating it to reflect industry best practices and regulatory shifts. Make improvement part of your workplace culture so everyone stays invested in seeing better results.
Building Your Path to Success
A denial management workflow that works isn’t about perfection. It’s about reliable execution, ongoing improvement, and removing chaos from your daily routine.
Combine smart prevention with systematic resolution, and let the right technology lighten your administrative load. Start small, maybe with a denial audit or automated alerts, then build from there. If you run into complex implementation issues or just want extra support, professional revenue cycle management services (like those from our team) can help you design a tailored workflow that fits your unique practice.
Remember: every improvement, no matter how small, contributes to a healthier revenue cycle and a more efficient team. With the right steps and a thoughtful approach, denial management can shift from a constant frustration into a strength that moves your practice forward.
