RCM
How to Bring Down the Denial Rate The Definitive Practical Approaches for Healthcare Professionals
Featured Post
The Top Denial Reasons by Insurance Payers and How to Boldly Outsmart Them
What We offer:
A denial rate as “low” as 5% can quietly drain away more than $150,000 a year from your practice. If you’ve ever felt stuck with high denial rates or thought it’s just an unavoidable part of the job, you’re definitely not alone. But here’s the good news: with the right systems and daily practices, we can bring those numbers down and reclaim revenue that’s too often written off.
Reducing denials isn’t just about getting claims paid; it’s about strengthening the whole revenue cycle in healthcare. What is RCM in healthcare? Revenue cycle management is about everything from a patient’s first interaction through the final bill being paid, and denial management is central to that process. By tackling the true causes of denials, we don’t just recover lost dollars; we also streamline daily operations and relieve stress for billing teams.
This post offers straightforward, actionable ideas for lowering your denial rate. We’ll look at the most common causes of denials, how to prevent them before they appear, and what it takes to keep those improvements going for the long haul, so your team can focus more on patients and less on paperwork.
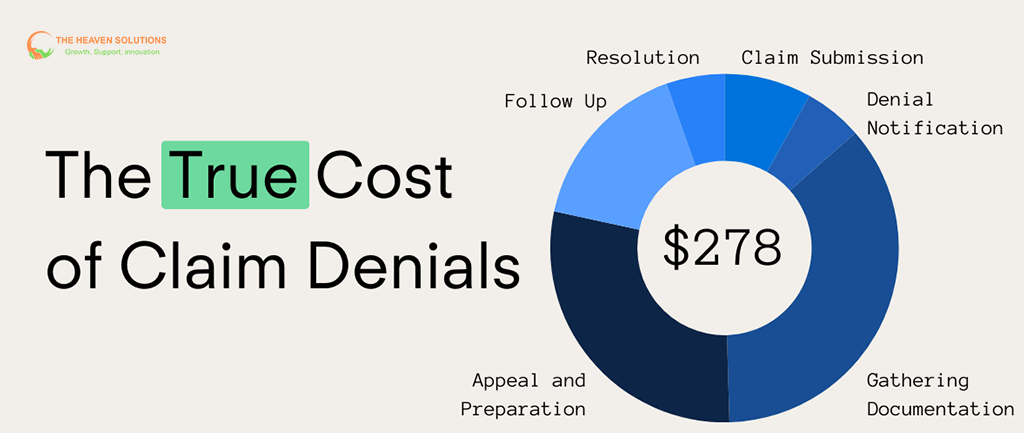
Denials do more than shrink your bottom line. Each denied claim costs time, creates extra steps for your team, and slows down your entire medical billing RCM process. Industry studies estimate each denial costs about $118 to resolve, but preventing one costs just $25–$30. Multiply that by hundreds or thousands of claims a year, and the expense grows fast.
Beyond that, staff who spend their days chasing denials have less time to help patients, manage follow-up care, or support practice growth. High denial rates can also mean more frustrated staff, unhappy patients waiting on claims, and slower cash flow for your organization.
Benchmarks vary, but most clinics and practices should aim for a denial rate under 8%. If you’re higher than that, there’s real room for improvement.

To fix denials, you need to know where and why they’re happening. Start by reviewing the past year of claim data. Track denials by month, payer, and reason. Most PMS or RCM systems can help you sort this info quickly. Create a report or spreadsheet that highlights denial counts, top reasons, payer sources, and the lost revenue attached to each.
Chances are, you’ll notice patterns: maybe a few denial types account for over half of your total, or one insurance payer denies far more claims than the rest. Rather than taking on everything at once, focus first on these highest-impact issues.
Many denials fall into the same categories over and over: front-end errors (like a simple typo or missing insurance info), missed authorizations, medical coding mistakes, or incomplete documentation. If you can cut these at the source, your numbers will improve across the board.
The majority of avoidable denials start at the very beginning with patient registration, eligibility checks, and authorizations. Get these right, and your claims are already on a smoother path.
Patient Registration: Double-check every detail at check-in. Use insurance card scanning, verify contact details, and confirm eligibility on the spot. Most modern RCM systems can verify benefits and coverage in real-time, catching problems early.
Authorizations: Automated tools can flag when prior auth is needed, or when a patient’s plan requirements have changed. Support your team with standard templates and built-in reminders. Schedule regular training sessions on the latest payer requirements, and have a plan to appeal auth denials quickly when they happen.
Referrals & Scheduling: Make it routine to validate every referral and network status before a patient sees a specialist. A simple phone call or electronic check can prevent out-of-network surprises and denied claims for missing referrals.
3- Level Up Documentation and Coding
Solid clinical documentation is your best friend for getting claims paid the first time. Templates for common procedures, detailed progress notes, and clear rationale for each care decision help support medical necessity and match payer policies.
When it comes to coding, specificity matters; ICD-10 and CPT mistakes are a leading cause of denials. Invest in ongoing training for your coding staff, use built-in validation or scrubbing tools in your billing software, and perform regular audits to catch issues before claims go out.
A strong revenue cycle management process puts coding accuracy front and center, not just to avoid denials, but also to help your team feel more confident in their work.
4- Let Technology Do the Heavy Lifting
Today’s RCM software, especially platforms that support seamless integration between EHR and billing, can automate many of the steps that keep denial rates down:
- Claims scrubbing identifies errors or incomplete fields before submission.
- Real-time analytics track trends, highlight recurring denial reasons, and benchmark performance against industry standards.
- Automated notifications alert staff about upcoming authorization expirations, recent payer policy changes, or claims that need immediate attention.
Be sure to select solutions that work with your clinical and billing workflow, not against it. The right tech lets your staff focus on the calls and claims that truly need a human touch.
5- Build a Prevention-Focused Culture
At the end of the day, lowering your denial rate is a team effort. Foster an environment where staff at every level, front office, clinical, billing, and management, know their role in preventing denials and feel empowered to flag issues.
Hold quick huddles or meetings to review denial rates, share wins, and talk through recent challenges. Recognize team members who catch errors before claims go out, and reward initiatives that prevent denials from happening in the first place.
Standardize processes with checklists and templates, and make ongoing training a routine part of your practice’s calendar. Keep everyone up to date on payer policies and use lessons learned from past denials to drive process improvements.
Keep the Momentum Going
Reducing your denial rate isn’t just a project; it’s a mindset that carries across your entire healthcare RCM journey. Continue to analyze your data monthly, adjust as payers and regulations change, and celebrate progress.
Scaling your efforts goes hand-in-hand with growth. As your practice sees more patients or expands services, revisit your prevention strategies. Make sure new team members receive training and that any new technology is supporting, not complicating, your workflow.
If you need to, seek support from RCM experts and industry partners who can share best practices or help set up a more automated, denial-proof workflow. Sometimes, an outside perspective makes all the difference.
Transform Your Practice's Financial Health Today
Navigating the challenges of revenue cycle management is a constant battle. Complex regulations, administrative burdens, and persistent claim denials can erode your revenue and distract you from your primary mission. The Heaven Solutions offers a comprehensive, expert partnership designed to overcome these obstacles. By combining specialized THS RCM services with powerful technology, we help you maximize revenue, reduce costs, and regain your focus.
Stop letting revenue slip through the cracks. Contact The Heaven Solutions today for a free consultation and discover how our partnership can transform your practice’s financial health.
