RCM
Appealing Denied Claims: A Comprehensive Step-by-Step Guide
Featured Post
The Top Denial Reasons by Insurance Payers and How to Boldly Outsmart Them
What We offer:

Getting a claim denial can be discouraging, especially when you know the service was both necessary and properly documented. You’re not alone. Many healthcare practices see denial rates in the 10–15% range, with certain payers pushing this even higher. The good news is, plenty of these denials can actually be appealed and won with the right approach.
Unfortunately, it’s common for appeals to be rushed and inconsistent. Too often, staff treat every denial as a one-off, not part of a larger pattern or process that can be improved. This guide is built for healthcare professionals looking for practical strategies to appeal denied claims confidently and improve their overall appeal systems over time.
You’ll learn how to analyze denial reasons, prepare strong appeals, work with different payers’ requirements, and turn what feels like busywork into a smarter, more reliable revenue recovery tool as part of your RCM (revenue cycle management).
Many practices lose out on appeals before they’re even filed. Why? Because poor prep, weak documentation, or missing deadlines can undermine an appeal, no matter how justified the claim.
Strategic Analysis Matters
Instead of jumping into writing an appeal letter, start with a careful review of the denial. What’s the actual reason code given by the payer? Does the appeal directly address that reason, or just repeat what was sent before?
Successful appeals start with a thorough analysis of what was submitted, checking against the payer’s explanation, and figuring out what needs to be added or clarified. In medical billing RCM, this step ensures you’re not leaving valuable revenue behind.
Strong Documentation Wins
Appeals rarely succeed if they just restate the original claim. If information was missing or unclear, the appeal needs to fill those gaps. Include any additional notes, clinical details, or supporting medical evidence that directly address the payer’s concerns.
Don’t Miss the Deadlines
Every payer has its own appeal window, some as tight as 30 days, others up to six months. Letting appeals slip can mean automatic loss even when you have a strong case. Tracking appeal deadlines is vital to the RCM cycle in medical billing.
To appeal a denial successfully, you have to know exactly why it was denied, and that means decoding the real message in the denial code.
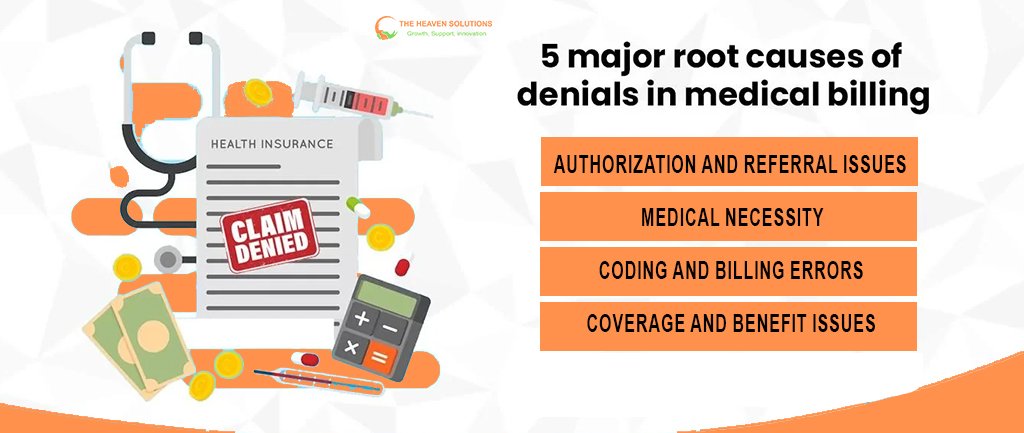
Common Denial Categories
- Authorization and Referral Issues: Denials for missing prior authorizations or referrals. Many can be resolved with clear proof that you followed the correct process.
- Medical Necessity: When payers question whether care was appropriate. These appeals need robust clinical notes and connections to established guidelines.
- Coding and Billing Errors: Simple errors in codes, mismatches, or missing modifiers. Some require claim corrections; others need clarified documentation.
- Coverage and Benefit Issues: Disputes about whether a service is covered or if a benefit was maxed out. These often need a deeper review of policy language and benefit interpretations.
Payer-Specific Patterns
Medicare, Medicaid, and commercial insurers each have their own habits and favorite denial types. For example, Medicare emphasizes documentation and medical necessity, while commercial payers may focus on authorization and network status.
Using your healthcare RCM software to track these patterns helps you spot trends and tailor your processes to prevent repeated denials.
The strongest appeals are built on thorough, organized prep:
Documentation Review
Start with all related documents: original claim, provider notes, test results, authorization records, and any payer communications. Check for incomplete or missing details, and create a timeline that logically connects care with the denied service.
Evidence Gathering
Add anything that wasn’t part of the first claim if it supports your position, like more detailed progress notes or supporting clinical research. Professional guidelines or peer-reviewed articles can back up your decisions, especially for medical necessity appeals.
Strategy Development
Shape your appeal around the denial type. For authorization issues, show documentation of the process or explain exceptional circumstances. For medical necessity, craft a patient-specific argument. Coverage disputes? Highlight contract language or plan benefits.
The appeal letter is your moment to make the case. Make it count:
Include:
- A summary of the claim and specific denial details.
- Your clinical rationale is clear, patient-centered, and tied to evidence or guidelines.
- Relevant supporting documents the payer hasn’t seen.
- A professional, straightforward request stating the outcome you want.
Tips:
- Structure the letter with clear headings and organized points to make it easy for the payer to follow.
- Reference payer-specific guidelines and requirements.
- Avoid angry or emotional language, stick to facts, and use a professional tone.
Every payer is different. Here are the basics:
Medicare Appeals
Features a multi-level process, starting with the MAC (Medicare Administrative Contractor) and moving, if needed, all the way to the Medicare Appeals Council. Know each level’s requirements and deadlines.
Commercial Payers
Typically offers both internal and external review processes. Use internal appeals for quick fixes or doc issues, escalate complex cases or clinical disputes to external review, often involving independent physicians.
Medicaid (State by State)
Medicaid appeals differ widely by state and by MCO. Know your specific process, whether it’s a fair hearing, a written review, or something else.
Advanced Appeal Strategies
If your standard approach isn’t working:
- Request a peer-to-peer review with the payer’s medical director
- Submit to independent medical review, especially for specialized or emerging care decisions
- File regulatory complaints if patterns of inappropriate denial appear (after documenting thoroughly)
Building Sustainable Appeal Systems
Long-term success in appeals depends on organized systems:
- Keep all appeal files and templates for easy reuse and documentation
- Track appeal outcomes by reason, payer, and approach, using your RCM systems
- Train staff regularly on payer policies and deadlines
- Set up workflows so no appeal falls through the cracks
- Monitor key metrics: appeal win rate, turnaround times, and financial impact
The Role of Technology in Appeal Management
RCM software and tools that integrate with your EHR and billing systems make it much easier to:
- Track appeals, deadlines, and outcomes
- Store documentation and version-controlled templates
- Analyze trends and performance for continuous improvement
Measuring Success and Continuously Improving
Monitor:
- Your appeal success rate (industry average: 60–70%)
- Time to resolution
- Shifts in denial and appeal fields over time
- Actual dollars recovered
And don’t forget regular debriefs, staff feedback, and payer communication sessions to keep your process agile.
Building Your Path to Appeal Success
Appealing denied claims doesn’t have to be a headache or a constant source of lost revenue. By treating appeal management as part of your larger medical billing RCM process, you can build a consistent, effective system that boosts cash flow and protects your practice.
Start by reviewing your most frequent denials and focus on one improvement at a time, whether updating documentation templates, stepping up staff training, or refining your use of RCMm software. And if your appeals feel unmanageable, Don’t hesitate to reach out for expert help or supportive services that fit your workflow.
A thoughtful, strategic approach to appeals will protect your revenue, reduce administrative headaches, and help ensure your practice gets paid for the care you provide.
