RCM
Fast-Track Your Reimbursement with Flawless Claim Submission
What’s Included
- Claims Submission & Follow-Up
- Denial Management
- Accounts Receivable (AR) Recovery
- Payment Posting & Reconciliation
- Patient Statements & Collections
- Clearinghouse Setup & Integration
Featured Post
The Top Denial Reasons by Insurance Payers and How to Boldly Outsmart Them
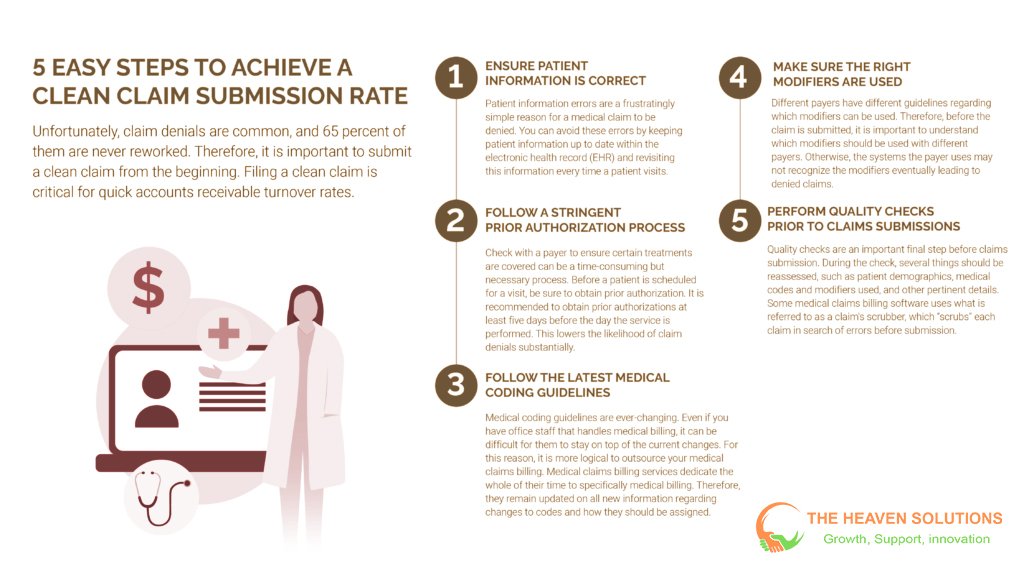
In the world of healthcare, the journey from providing patient care to getting paid can feel like a marathon. But what if there was a way to turn that marathon into a sprint? The secret isn’t running faster; it’s starting with a flawless first step: accurate claim submission. At the heart of every healthy revenue cycle is the concept of a “clean claim,” a claim submitted to an insurance payer that is error-free.
These error-free submissions are the key to a healthy revenue cycle management process. This post will break down why claims processing accuracy is so critical, identify the common errors that cause costly delays, and provide actionable tips to help your practice achieve a higher clean claim rate and accelerate your cash flow.

The Anatomy of a Clean Claim Submission: Why Accuracy Is Everything
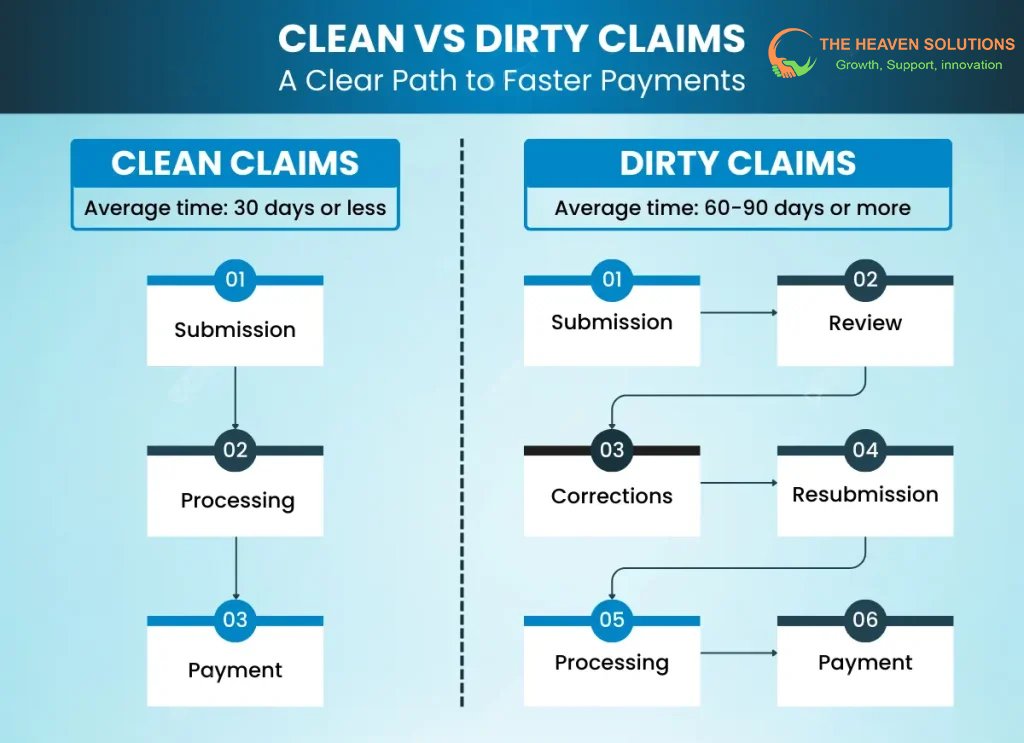
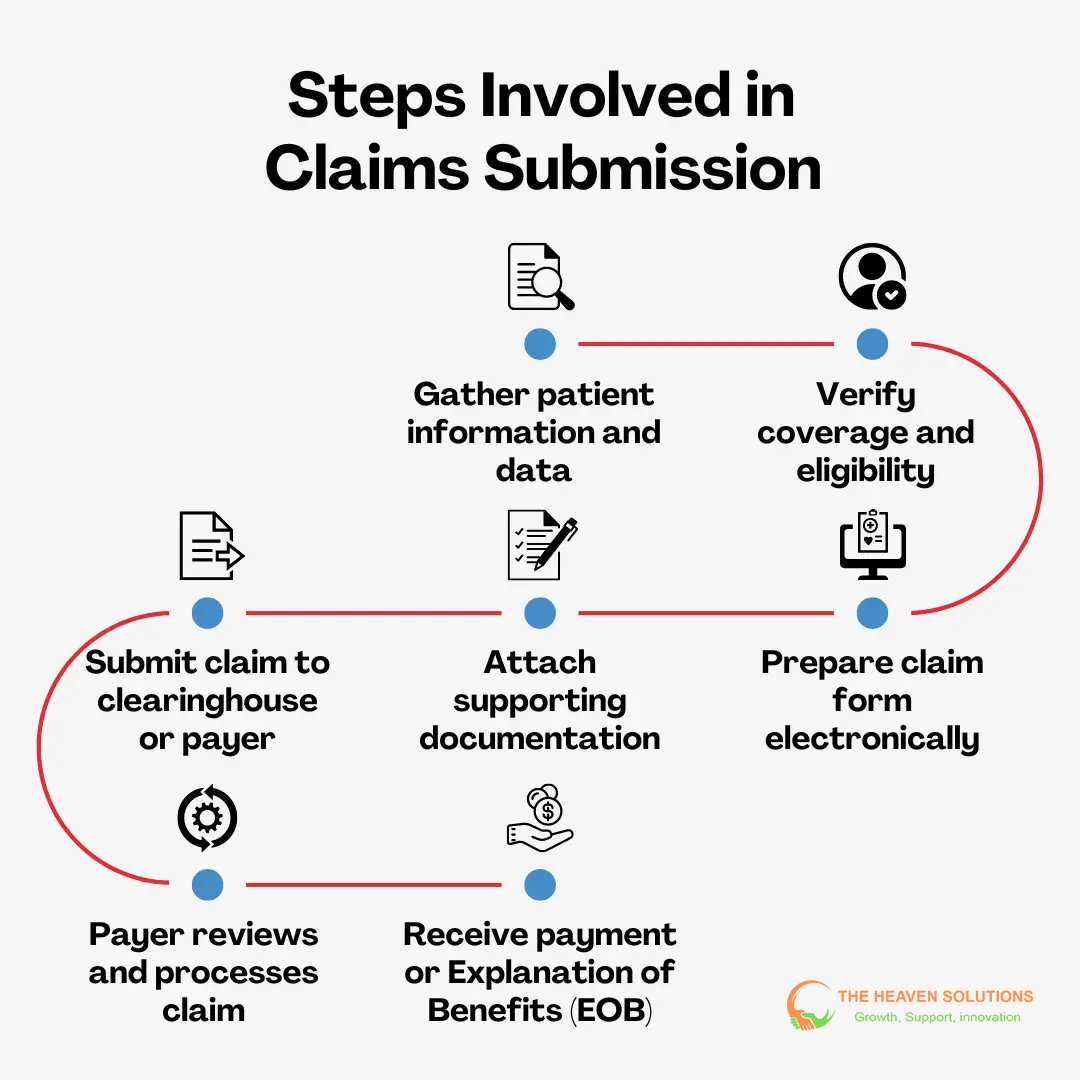
So, what is a clean claim in medical billing? A clean claim is an error-free insurance claim that is submitted electronically and can be processed by the payer’s system without requiring any manual intervention. The direct correlation between a high clean claim rate and a short payment cycle is the foundation of efficient RCM in medical billing.
Contrast this with “dirty claims,” which contain errors and immediately enter a frustrating cycle of rejection, rework, and resubmission. Think of it this way: a clean claim is like a non-stop flight, reaching its destination quickly and efficiently. A dirty claim is a flight with multiple layovers, unexpected delays, and a high likelihood of being delayed or lost.
The difference in timing is significant. Clean claims are often processed and paid within 14-30 days. A claim with even a minor error can take 60, 90, or even more days to resolve, wreaking havoc on your practice’s financial stability. Effective healthcare revenue cycle management is about maximizing the number of non-stop flights and minimizing turbulence.
Common Roadblocks: Top Errors That Delay Payments
Understanding the most frequent errors is the first step toward improving your claim submission in medical billing. These common roadblocks are what turn a straightforward claim payment into a lengthy and expensive follow-up project.
Patient Information Errors
These are some of the most common yet preventable mistakes. Simple clerical errors made at the front desk can stop a claim in its tracks.
- Examples: Misspelled names, an incorrect date of birth, invalid insurance ID numbers, or an outdated address. If the patient’s data on the claim doesn’t perfectly match the payer’s records, it will be rejected.
Medical Coding and Service Errors
The services you provide must be translated accurately into the language of medical codes. This is a frequent source of claims processing issues for many practices.
- Examples: Use of outdated or non-specific ICD-10 or CPT codes, mismatched diagnosis and procedure codes that fail to establish medical necessity, or the incorrect use of modifiers.
Insurance and Authorization Errors
Finally, errors related to the payer and pre-approvals are a guaranteed cause for delay.
- Examples: Submitting the claim to the wrong insurance company, providing services that required prior authorization but were never obtained, or billing for services that are not covered under the patient’s specific plan.
The Ripple Effect: Benefits Beyond Faster Payments
The importance of revenue cycle management and accurate claims goes far beyond just getting paid faster. The positive effects ripple throughout your entire practice, improving operations, finances, and the patient experience.
Reduced Administrative Costs
Accurate claims require significantly less staff time. When a claim is submitted correctly the first time, your team spends less time on hold with insurance companies, writing appeal letters, and reworking rejections. This dramatically lowers your overall cost to collect and frees up your staff to focus on more value-added activities, like patient care.
Improved Cash Flow and Predictability
A consistent flow of clean claims creates a stable and predictable revenue stream. This is one of the most significant benefits of revenue cycle management. When you can accurately forecast your monthly income, you can make better business decisions, manage expenses with confidence, and plan for future growth.
Enhanced Patient Satisfaction
Claims processing accuracy directly impacts your patients. When claims are processed correctly, patient statements are accurate. This prevents surprise bills and reduces the number of confused and frustrated phone calls to your front desk. A smooth financial experience is a crucial part of overall patient satisfaction and retention.
Actionable Data Insights
When your claims processing is accurate, you can trust your financial data. This allows your revenue cycle manager to analyze performance and easily identify positive or negative trends. You can pinpoint profitable service lines or identify the root cause of recurring issues, empowering you to make informed, data-driven decisions to optimize your practice.
Conclusion
Accurate claim submission is the foundation of a healthy revenue cycle in healthcare. It’s not just an administrative task but a core strategic function. By creating a workflow that avoids common errors related to patient, provider, and service information, practices can generate clean claims that get paid faster and with less effort.
Investing time and resources into accuracy upfront pays significant dividends. The result is reduced administrative costs, dramatically improved cash flow, and a better financial experience for your patients. It’s the most direct path to a stronger, more stable practice.
Don’t let preventable errors slow down your revenue. Contact The Heaven Solutions today for a complimentary claim analysis. Our experts can help you identify the root cause of your denials and build a streamlined submission process that accelerates your payments.
